Why should your medical credentialing be outsourced?
Medical credentialing and insurance enrollment are the initial barriers to receiving timely payments in revenue cycle management. Every medical practice, regardless of size, faces a daily onslaught of hurdles aimed at preventing or limiting reimbursement for services. This should come as no surprise if you’ve been in business for a while, and you may have contemplated outsourcing your credentialing to the best medical credentialing companies. As you are probably aware, insurer credentialing or provider enrollment has become one of the most convoluted and perplexing processes in the healthcare sector over the years.
Healthcare facilities, as you are all aware, exist to facilitate and give medical treatment to their patients. While we have evolved like never before in our curative procedures, infection prevention, illness control, and practically every other measurable parameter, the obstacles to maintaining a profitable practice have only grown in scale.
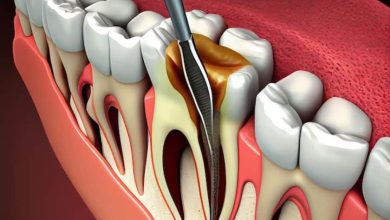
What Exactly Is Provider Medical Credentialing?
Provider credentialing is the process through which medical organizations and insurance companies validate healthcare professionals’ credentials to ensure they have the necessary licenses, qualifications, and abilities to care for patients. Physician credentialing, medical credentialing, and doctor credentialing are all terms used to describe the procedure.
Why Do Medical Billing Firms Encourage Medical Credentialing?
In the healthcare business, quality of care has taken center stage; every stakeholder employs cutting-edge ways and procedures to attain this goal. Wherever technology is unavoidable, the medical staff’s experience is also required to treat patients properly. It also increases the income of the medical practice.
We cannot, however, call into question the medical staff’s integrity. Furthermore, hospitals today have a proclivity for medical billing qualifications. Nobody now will overlook credentials at any health facility, including outpatient centers, long-term care facilities, and emergency clinics.
Build a sense of trust and confidence between physicians and providers based on the qualifications of health practitioners, patients, and healthcare providers. In the past, we have seen several examples of bogus grads managing patents. Such carelessness has no place in today’s environment, especially after the epidemic.
This article will teach you how to perform professional credentials. The criteria and credentials feature has undoubtedly become more sophisticated over time. That must be due to the provider’s and accrediting organizations’ reach and standards. Top medical billing companies will use specialized tools and processes to expedite the process, giving your workers more time to focus on patient care and support.
Here are some critical responsibilities that will persuade you to outsource medical credentialing and enrollment to a competent medical billing and coding company.
Specialized services are provided
Some functions at a healthcare institution need specialized training and skill sets, which is where outsourcing comes in. IT administration tasks are often at the forefront of this category since not many practices, particularly small facilities, can afford a full-time IT employee.
Credentialing falls into this category because it is a one-of-a-kind service that necessitates someone with expert knowledge of the processes in order to successfully maintain your medical credentials with hospitals, insurance plans, and other healthcare organizations that require provider credentialing. When handled improperly, it can have a significant influence on your revenue cycle.
Work that is repetitive
Because of the repetitive nature of completing insurance credentialing and enrollment for physicians. As well as the follow-up required to finish the process with payers, this job is a great candidate for outsourcing. The daily activities of document maintenance, updating patient profiles, and continuing credential checking are time demanding and should be left to someone with automation and a special emphasis on these duties.
Requires expertise in the job
Hiring medical billing and coding professionals in a business function outside of your main job area is frequently a wise decision since those services are best suited for outsourcing. Practices focused on delivering professional healthcare services do not need to recruit, retain, or manage certifying specialists. They can outsource these tasks directly to partners whose primary skill and business is certification. The credentialing professionals can assist you in strengthening your revenue cycle management by ensuring that your providers are registered in health plans on time.
Remember that medical credentialing and enrollment are suitable for outsourcing. Any healthcare facility should consider outsourcing this activity to a business partner whose primary business is credentialing and enrollment.
The true worth of your time
While credentialing is a price in and of itself, the true cost of credentialing is the time a physician is working – or not working. A delay in credentialing might result in time away from work or from seeing patients with certain insurances. The cost of missed income due to delays can potentially exceed the cost of credentialing itself. Credentialing can potentially take a long time, especially if things go wrong. Physicians frequently undervalue their own time. And the last thing you want to do is wait for a credentialing agency to contact you back.
Read more blogs about Medical Billing and Credentialing